
Content derived from “Understand the Signs, Symptoms, and Prevention of Stroke”
A virtual town hall with neurologist, Dr. Michael Previti on September 24, 2021.
What is a stroke and why is preventing one important?
A stroke is a like a “heart attack of the brain.” Because everything in your body needs blood to live, your organs have blood vessels that supply them with blood which allows them to function. If a blood vessel becomes blocked, then it can’t get the blood it needs and it starts to die. When your heart isn’t getting enough blood, it dies, and that’s a heart attack. When your brain isn’t getting enough blood, it dies, and that’s a stroke.
This is important because stroke is the second leading cause of death worldwide and it’s the number one reason people become disabled in the United States when they’re of working age or older. If we have an understanding of what causes stroke, we’re less likely to have one. If we know what it looks like, we can call 9-1-1 as soon as possible, because every minute matters. Having a stroke can be devastating if things go wrong, but they don’t have to! I like to say that an ounce of prevention is worth a pound of cure. The better we can understand what puts us at risk for poor outcomes, the better we can work against those outcomes.
How do blood vessels become blocked?
A blood vessel refers to both your arteries and your veins because they both carry blood throughout your body. The heart pumps blood up to your brain inside arteries and sometimes, those arteries get blocked. Sometimes, these blockages come from the heart when it is not pumping well. This can happen because of an irregular heart rhythm, an old injury to the heart, like a heart attack, or if there is any other damage to the heart itself. This damage can cause a clot to form in the heart, which can travel up to the brain and block the blood vessel.
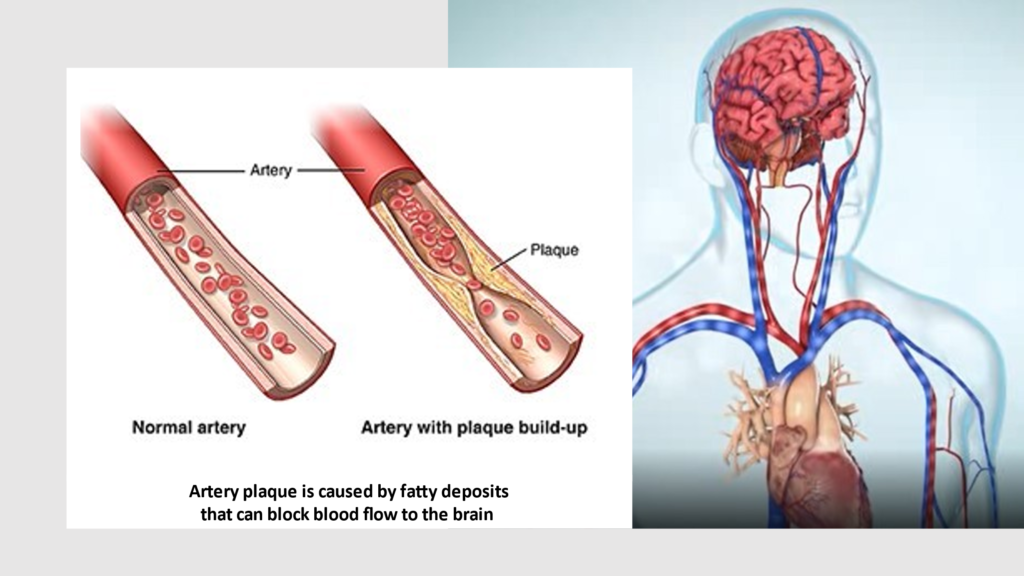
In addition to a clot, a stroke may also occur because of plaque build-up in the blood vessels. If you’ve ever seen the inside of partially clogged house pipe with a crust built-up around the inside edges, that is what is happening inside the blood vessels when plaque builds up. The more plaque builds-up in the blood vessel, the more difficult it is for the blood to flow.
How do you treat blocked arteries?
To treat a blocked artery, we try to open up the blockage. We can do this in two different ways:
- Blood Thinner: We can administer a strong blood thinner, tissue plasminogen activator, known as tPA. This medication works really well, but the sooner you give it, the better. For example, if tPA is given within 60 minutes from when a stroke starts, patients have a 50% chance of getting better. If it’s given within 180 minutes from when the stroke starts, those chances reduce to about 14%. Once four and a half hours have passed, this treatment is no longer beneficial. tPA is the best medicine to treat 90% of all strokes.
- Surgical Removal: Another option, if the blockage is large, is to go in and surgically remove it. This is a minor surgery, and the good news is, it works very well. The downside to this procedure is that the blockage has to be a certain size to qualify for surgical removal, but 90% of blockages associated with stroke are too small.
What puts a person at risk for a stroke or blocked blood vessel?
There are several different risk factors for stroke, and they all affect the health of our blood vessels. These risk factors tear up your blood vessels, similar to cutting your skin, and just like your skin, when the wound begins to heal, it forms a scab. The difference is that the inside of your body takes a lot longer to heal because blood is constantly rushing through it. To make up for that difference, your body tries to cover up the scab with cholesterol, also known as plaque.
Over time, with each additional risk factor added, the plaque gets a lot bigger. Every cigarette, every bit of processed food, having uncontrolled diabetes, exposure to air pollution–each occurrence cracks open that scab. Then the scab bleeds again, and your body puts another scab on top of that, and more cholesterol on top of that. Each time, this reduces the amount of space for your blood to flow throughout the vessel.
What are the top five risk factors for stroke?
- High blood pressure
When someone has high blood pressure, it means they have a lot of pressure pushing against the wall of their blood vessels. Blood vessels are made of muscle, and muscles only know how to do one thing: push back. This means that when pressure is pushing up against the side of your blood vessel, it pushes right back. Similar to how we build muscle with exercise, this causes the wall of your blood vessel to thicken, reducing the amount of space for your blood to flow. This decrease in space for blood flow becomes even more important when we add in the plaque build-up that further reduces the available space. All of this means that in the instance of stroke prevention, high blood pressure is the number one enemy–and in South King County, high blood pressure is twice the national average. - Tobacco use
The chemicals inside tobacco damage your blood vessels, causing high blood pressure, and we know why that’s bad! The best way to get a handle on it is to remove the risk factor altogether—this means no smoking, chewing, or ingesting tobacco products. - Processed foods. Bacteria and fungus like to eat our food which causes the food to spoil. Packaged foods have preservatives in them that kill bacteria and fungus on contact, preventing the food from going bad too quickly. This allows us to ship food across the world and have it still be okay to eat when it gets there. However, those preservatives are full of things like salt, sugar, and other chemicals, which are are toxic to cells. So, while preservatives keep bacteria and fungus from getting to our food, they also cause significant damage to our blood vessels.
- Diabetes
Similar to how the sugars in preservatives can affect your blood vessels, when blood sugar levels become too high in the body, this can also damage your blood vessels. When blood sugars are out of control, it increases your risk for stroke by two to six times.
The average person has about a 2% risk of having a stroke. If someone has high blood pressure that puts them at an 80% risk, and on top of that, if their blood sugar is out of control, that continues to increase their risk of having a stroke. - High cholesterol
Now that we see how the body uses cholesterol to cause plaque buildup inside the blood vessels, similar to scabs on our skin, we can better understand why it’s important to keep your cholesterol levels under control—cholesterol plays a big role in restricting the flow of blood through your vessels. When you get your cholesterol checked, there are a lot of numbers in that panel. The one that matters most is known as your LDL, L for lousy. We want to keep that number below 70.
Does age affect your risk for stroke?
Yes, age does matter. It matters because while everyone is at risk for a stroke, it’s our levels of risk that vary. When you’re young, your risk is lower, and when you’re older, your risk is higher. The age at which we commonly see strokes often depends on lifestyle. If you move your body regularly, eat fairly well, and don’t have high blood pressure, you might be at your highest risk for stroke in your 70s or 80s. If you smoke cigarettes, aren’t terribly active, and also have high blood pressure and/or diabetes, you might experience a stroke in your 40s or 50s.
What does a stroke look like and what do I do if someone is having one?
Recognizing the signs of a stroke is so important it has its own acronym, F.A.S.T.
Face – Is their face drooping on one side? Can they only move one side of their face? Their face doesn’t look the same on both sides.
Arms – Can they lift and operate both arms normally? They should be able to hold their arms out in front of them, like they’re holding a bowl.
Speech – Is their speech slurred, difficult to understand, not making sense, or are they completely unable to speak at all?
Time – As soon as you see any of these symptoms, DON’T WAIT, call 9-1-1 immediately.
Each of these recognition points is important, but time is crucial. Every minute of a stroke, 2 million brain cells die. Don’t wait to see if it’s going to get better. As soon as you see the face is uneven, the arms aren’t working evenly, and the speech is abnormal, call 9-1-1. The sooner we can treat it, the sooner we can stop the cell death.
Other than calling 9-1-1, it can be helpful to always keep a list of your medications with you in case something happens. Additionally, have conversations with your family about your health history and important healthcare decisions in case of an emergency. Your healthcare team will also want to know when the symptoms started or the last time someone saw you perfectly normal.
What does recovery after a stroke look like?
In the first 24 hours after a stroke, we’re doing everything we can to make your symptoms better. Once your symptoms are under control, we’re trying to figure out what caused your stroke. Since we know that blood clots from the heart can be one of the causes, we’re going to evaluate your heart and all those other factors we’ve talked about. We’ll perform tests, assess your heart rhythm, check for diabetes, high cholesterol, and high blood pressure, we’ll look at the plaque in your blood vessels, and we’ll look at your brain. Having all this information allows us to come up with a treatment plan that will reduce your risk of having another stroke as much as possible.
At Valley, we have a Stroke Clinic that I’m very proud of. When someone comes to us to treat a stroke, our goal is to get them out of the hospital and into the clinic in 7-14 days. For the next couple of months, we focus on a stroke plan of care and finding the right medication levels. This is where we focus on reducing your risk factors, like making sure your blood pressure, blood sugar, and cholesterol are stable. Each reduced risk factor reduces your likelihood of having another stroke.
Some may also need rehab after a stroke. Everyone’s brain is different, and each stroke is different, so everyone’s deficits after a stroke are also going to be different. Some people are lucky enough to leave the hospital almost completely free of symptoms and without the need for rehab, but not everyone falls into that category. In fact, most people don’t. More commonly, after a stroke, people need rehab, which can include a lot of options.
- Home Health: Home health is rehab therapy you get to do at home. This is often an option for those who are doing so well that it makes sense for them to go home, but they still need someone with them, for support, 24 hours a day. Therapists will visit the home a few times a week to help work on recovery. Depending on your symptoms, this may include physical therapy for walking, occupational therapy for improving the use of your arms and hands, or speech cognitive therapy for help speaking and/or swallowing.
- Inpatient Rehab: This is for patients who can’t safely go home. Inpatient rehab often includes a hospital-like facility where patients commonly stay for 2-4 weeks. Everyone is different, so the length of stay will depend on the severity of your symptoms and how well you respond to treatment. This therapy can be intense, but it’s worth it. During this time, patients participate in the various types of therapy for about three hours every day.
Starting therapy as soon as possible is important because after the brain is damaged, it tries really hard to repair itself from that damage, but only for a short window of time. Eventually, the brain will decide that if it has not repaired itself by now, it’s not going to happen, and then therapy is no longer effective. - Short-Term Rehab: This is for people who can’t manage therapy for three hours a day for 2-4 weeks. Instead, patients in short-term rehab are often doing therapy for about an hour each day, for three to five days a week. The therapy is a lot less intense, but these people often need a lot more help. Short term rehab is for people who have disabling symptoms that require them to need a lot of help with mobility, support getting to and from the bathroom, and changing their clothes. Unfortunately, most people need short-term rehab after a stroke.
- Long-Term Care: This is rare, but sometimes a stroke can disable someone so severely that none of these other options work and they are moved to a nursing home. In these instances, patients need skilled and significant help all day long and this is what we are trying to avoid.
Post-stroke issues have an enormous range, but commonly, people are really tired all the time and can have difficulty concentrating. This is common because they’ve just lost a part of their brain. Imagine if you had 100 employees, and five of them got laid off, and now your remaining 95 employees must work harder to get the same amount of work done, with less people. This is what is happening in the brain after a stroke; you lose part of your brain, so the rest of your brain must work harder, and it gets exhausted. This means people often need more sleep or to take naps in the middle of the day, but your brain needs that rest to heal, and after about six months, these problems start to get significantly better.
Are there tests my doctor could do that would help to predict my likelihood of having a stroke?
Absolutely! Your physician can assess those five primary causes or risk factors for stroke. They can check your blood pressure, and your blood sugar and cholesterol levels. Talking to your doctor about the risk factors specific to you is the best way to create a plan that will reduce your risk as much as possible. They can tell you your cholesterol levels, whether you have diabetes, and they can show you how to keep track of your own blood pressure.
If you have a strong family history of plaque buildup in the blood vessels, you could have them looked at using an ultrasound, to see if you have any. Then, if you know you have plaque already built up, you can be more aggressive in combating it.
What can I do to reduce my risk of stroke?
You reduce your risk for stroke by making changes to your lifestyle that you know will reduce the amount of plaque buildup in your blood vessels. Making these changes can drastically decrease your risk of having a stroke and all the associated hardships that come with it; they are:
No tobacco or alcohol
- Avoid them in any form (i.e., smoking, vaping, chewing, or ingesting of any kind).
Change your diet
- Don’t eat processed foods.
- Focus on eating vegetables, fruits and nuts.
- Avoid butter, use oil instead.
- Avoid cured meats (anything that can sit out in the sun).
- When it comes to meat, anything that comes from the ocean is better than anything from the air, which is better than anything that comes from the land. Red meat is particularly bad.
- Eating well matters more than how much you eat, because when you eat well, it creates good bacteria in your gut, which leads to better blood vessel health.
- Stop eating two hours before you go to bed.
Control your blood sugar
- If you have Diabetes, we’re looking at a number called an A1C. This measures a person’s average blood sugar levels over the past three months. Our goal is to keep that number as low as possible and to keep your blood sugar normal, around 80 to 100.
Monitor your blood pressure
- Blood pressure is read using two numbers, a top number, and a bottom number. The top number is known as your systolic blood pressure and the bottom number is known as your diastolic blood pressure. Commonly, you’ll see numbers like 120/80, and our goal is to keep your blood pressure below those numbers. Unfortunately, most people in South King County are walking around with a systolic blood pressure closer to 140 or 150.
- This is important because every 10 points above 120 increases your risk for stroke by 41%. This means that if your top number is 140, you have a 68% increased risk of stroke. If it’s 150, that’s an 80% increased risk—it adds up really fast!
- This is why we recommend checking your own blood pressure on a regular basis. If it’s not less than 130/80 80% of the time, you should see your doctor.
Move your body
- Move your body as much as possible.
- Go for a 15-minute walk after every meal.
Get good sleep
- The average person needs 7 to 9 hours of sleep a night.
- Deep sleep is when your body clears out toxins and repairs damage, so sleep is how your body repairs the plaque in the blood vessels.
- REM sleep is when your body reorganizes all the information you’ve learned–this is when you experience dreams.

